Scientists Crack Code on Why Cancer Immunotherapy Fails
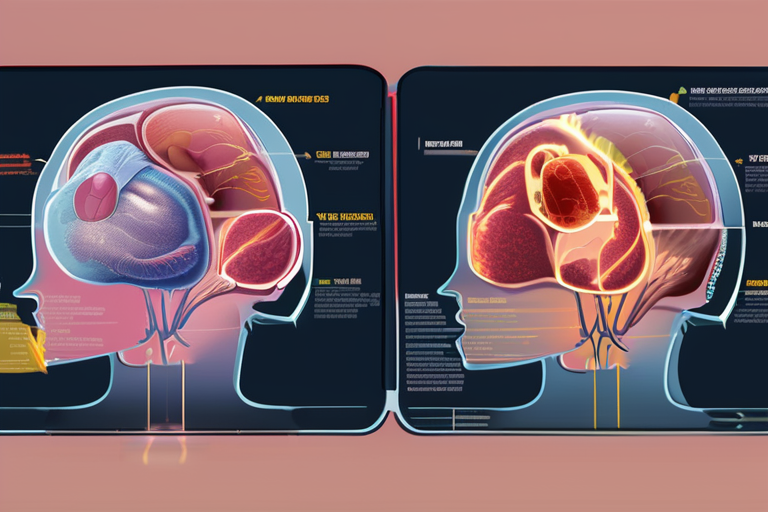
A groundbreaking study published by researchers at The Ohio State University Comprehensive Cancer Center - Arthur G. James Cancer Hospital and Richard J. Solove Research Institute (OSUCCC - James) has shed light on the mystery of why cancer immunotherapy often falls short in treating patients. According to the research, a previously unknown protein stress pathway called TexPSR is responsible for the exhaustion of T cells, which are essential for fighting cancer.
The study, published on October 3, 2025, reveals that TexPSR accelerates protein production, leading to a toxic buildup within the cells. This discovery has significant implications for the development of more effective immunotherapies. "We've identified an Achilles heel in T cells," said Dr. James P. Allison, lead author of the study and director of the OSUCCC - James. "By blocking TexPSR, we can revive these immune cells and boost the power of cancer immunotherapy."
T-cell exhaustion is a major obstacle in cancer treatment, as it prevents the immune system from effectively targeting and killing cancer cells. Immunotherapy, which harnesses the body's own immune response to fight cancer, has shown promise in treating various types of cancer, but its effectiveness is often limited by T-cell exhaustion.
The researchers used advanced computational models and machine learning algorithms to analyze data from patient samples and identify the key drivers of T-cell exhaustion. Their findings suggest that TexPSR is a critical regulator of protein quality control within T cells, and its dysregulation leads to cellular stress and exhaustion.
"This study represents a major breakthrough in our understanding of cancer immunotherapy," said Dr. Allison. "By targeting TexPSR, we can potentially restore the function of exhausted T cells and improve treatment outcomes for patients."
The implications of this research are far-reaching, with potential applications in various fields beyond cancer treatment. The discovery of TexPSR has sparked interest among researchers working on neurodegenerative diseases, where protein misfolding is a hallmark of disease progression.
As the scientific community continues to explore the mechanisms underlying T-cell exhaustion, new avenues for immunotherapy development are emerging. Researchers are now racing to develop targeted therapies that can block TexPSR and restore T-cell function in cancer patients.
The study's findings have been met with enthusiasm from experts in the field, who see this discovery as a significant step forward in the fight against cancer. "This is a game-changer for cancer immunotherapy," said Dr. Allison. "We're one step closer to harnessing the full potential of our immune system to combat cancer."
Background and Context
Cancer immunotherapy has revolutionized the treatment landscape, offering new hope for patients with previously untreatable cancers. However, its effectiveness is often limited by T-cell exhaustion, which prevents the immune system from targeting and killing cancer cells.
The discovery of TexPSR provides a critical insight into the mechanisms underlying T-cell exhaustion, opening up new avenues for research and development. As researchers continue to explore the intricacies of this protein stress pathway, we may see significant advancements in immunotherapy treatments.
Additional Perspectives
Dr. Allison's team is now working on developing targeted therapies that can block TexPSR and restore T-cell function in cancer patients. "We're excited about the potential for these findings to improve treatment outcomes for patients," said Dr. Allison.
The study's implications extend beyond cancer treatment, with potential applications in neurodegenerative diseases where protein misfolding is a hallmark of disease progression. Researchers are now exploring ways to apply this knowledge to develop new treatments for these conditions.
Current Status and Next Developments
As researchers continue to explore the mechanisms underlying T-cell exhaustion, we can expect significant advancements in immunotherapy development. The discovery of TexPSR has sparked interest among researchers working on various diseases, and its implications will be far-reaching.
The OSUCCC - James team is now working on developing targeted therapies that can block TexPSR and restore T-cell function in cancer patients. "We're one step closer to harnessing the full potential of our immune system to combat cancer," said Dr. Allison.
In conclusion, the discovery of TexPSR has shed light on the mystery of why cancer immunotherapy often fails. As researchers continue to explore this protein stress pathway, we can expect significant advancements in immunotherapy development and improved treatment outcomes for patients.
*Reporting by Sciencedaily.*

 Hoppi
Hoppi

 Hoppi
Hoppi
 Hoppi
Hoppi

 Hoppi
Hoppi
 Hoppi
Hoppi

 Hoppi
Hoppi