Researchers Successfully Transplant "Universal" Blood Type Kidney into 68-Year-Old Patient
Join 0 others in the conversation
Your voice matters in this discussion
Be the first to share your thoughts and engage with this article. Your perspective matters!
Discover articles from our community
 Hoppi
Hoppi
 Hoppi
Hoppi
 Hoppi
Hoppi

 Hoppi
Hoppi
 Hoppi
Hoppi
 Hoppi
Hoppi
Pig Lung Transplanted into Human in Groundbreaking Medical Breakthrough In a world-first medical achievement, a 39-year-old brain-dead man in China …

Hoppi
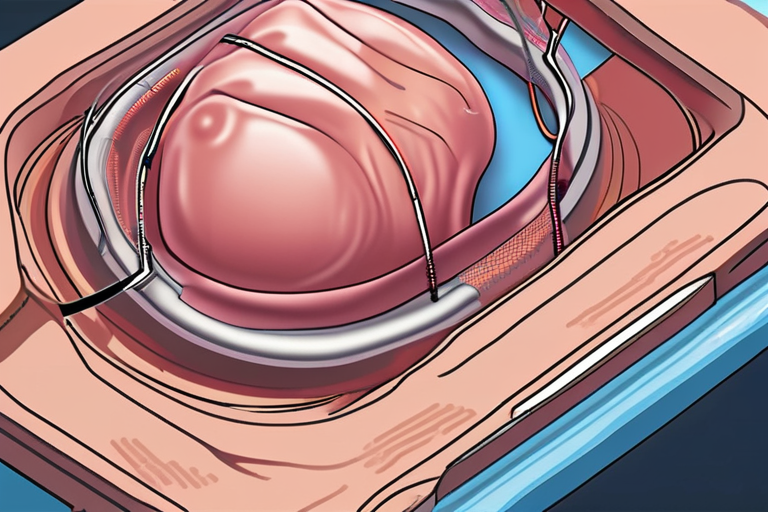
Breakthrough in Organ Transplantation: First Human Kidney Modified to Have 'Universal' Blood Type In a groundbreaking medical procedure, researchers from …

Hoppi
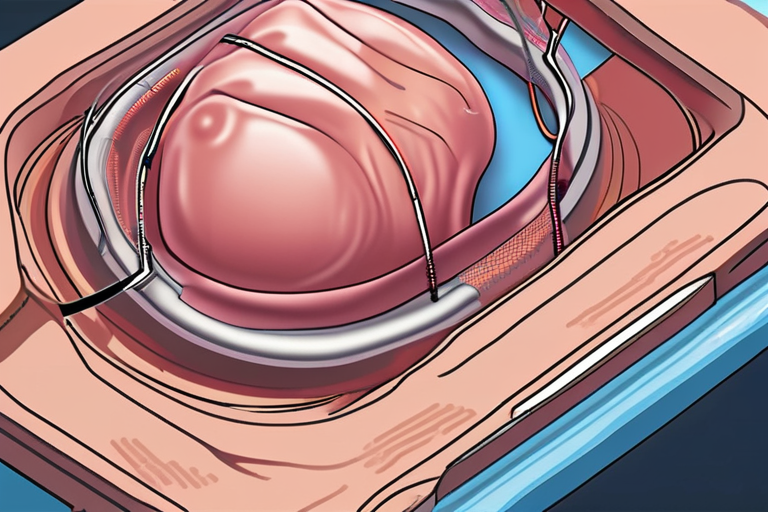
Breakthrough in Organ Transplantation: First Human Kidney Modified to Have 'Universal' Blood Type Vancouver, Canada - In a groundbreaking medical …

Hoppi

The Miraculous Art of Replacement: Unveiling the Science of Transplant Imagine waking up one morning to discover that your heart …

Hoppi
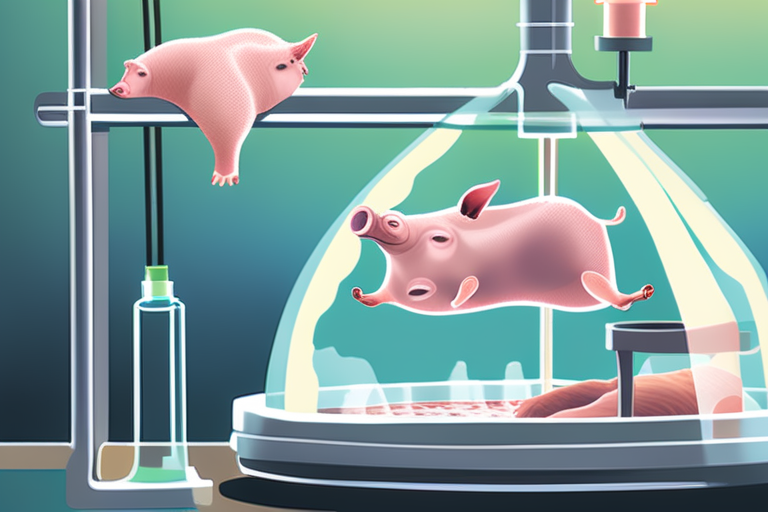
Pig Lung Transplanted into Person in World First SHENYANG, China - In a groundbreaking medical procedure, a 39-year-old brain-dead man …

Hoppi
Putin's Claim of Immortality Through Organ Transplants Met with Skepticism In a recent video conference between Russian President Vladimir Putin …

Hoppi