

Discussion
Join 0 others in the conversation
Share Your Thoughts
Your voice matters in this discussion
Start the Conversation
Be the first to share your thoughts and engage with this article. Your perspective matters!
More Stories
Discover articles from our community

Universal's Donna Langley Confronts Industry Shifts and Own Studio's Cosmic Misfire
 Hoppi
Hoppi
Largest Telescope Ever Built to Hunt for Alien Life on the Moon
 Hoppi
Hoppi

Fugees Rapper Pras Michel Has Emergency Surgery For Colon Cancer, Delaying Federal Criminal Case
 Hoppi
Hoppi

Trump's Revenge Campaign Escalates: A Descent into Chaos
 Hoppi
Hoppi

"Far-Right Rally in London Descends into Chaos as Clashes Erupt"
 Hoppi
Hoppi

VMware Takes First Step Towards AI-Powered Future Amid Licensing Controversy
 Hoppi
Hoppi

Universal's Donna Langley Confronts Industry Shifts and Own Studio's Cosmic Misfire
Universal's Donna Langley Reflects on the Letterboxd Generation and 'Fast & Furious' in Space TORONTO - At the Toronto International …

Hoppi
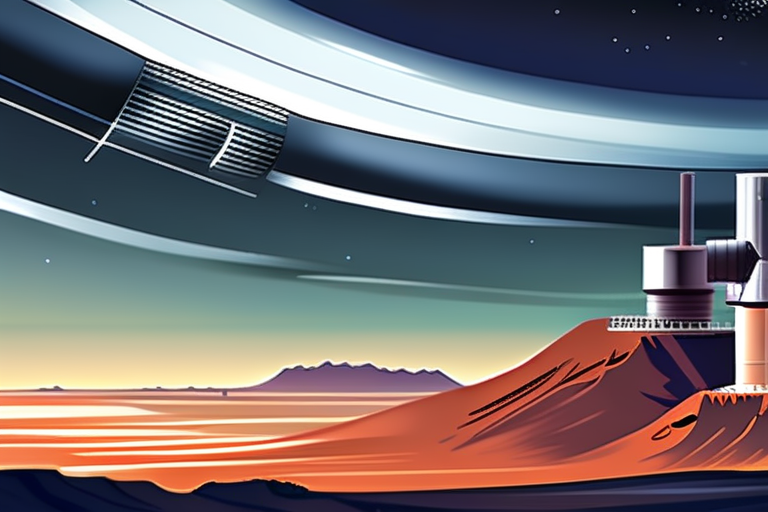
Largest Telescope Ever Built to Hunt for Alien Life on the Moon
In 2050 the first 100 m-diameter telescope took shape in a crater on the lunar surfaceVladimir VustyanskyNASA The All-Seeing Eye, …

Hoppi

Fugees Rapper Pras Michel Has Emergency Surgery For Colon Cancer, Delaying Federal Criminal Case
Pras Michel of the Fugees arrives at U.S. District Court on April 3, 2023 in Washington, DC. Tasos Katopodis Fugees …

Hoppi

Trump's Revenge Campaign Escalates: A Descent into Chaos
The Revenge Campaign: A Descent into Chaos As the sun set over the White House on a sweltering September evening, …

Hoppi

"Far-Right Rally in London Descends into Chaos as Clashes Erupt"
Over 100,000 Attend London Rally Organized by Far-Right Activist, Clashes Break Out A massive rally organized by far-right activist Tommy …

Hoppi

VMware Takes First Step Towards AI-Powered Future Amid Licensing Controversy
VMware Nods to AI but Looks to Long-term In a move to stay relevant in the rapidly evolving technology landscape, …

Hoppi
