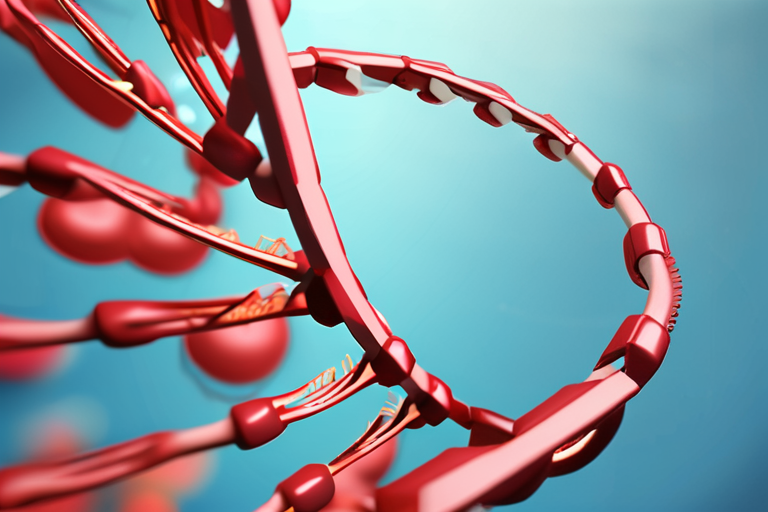
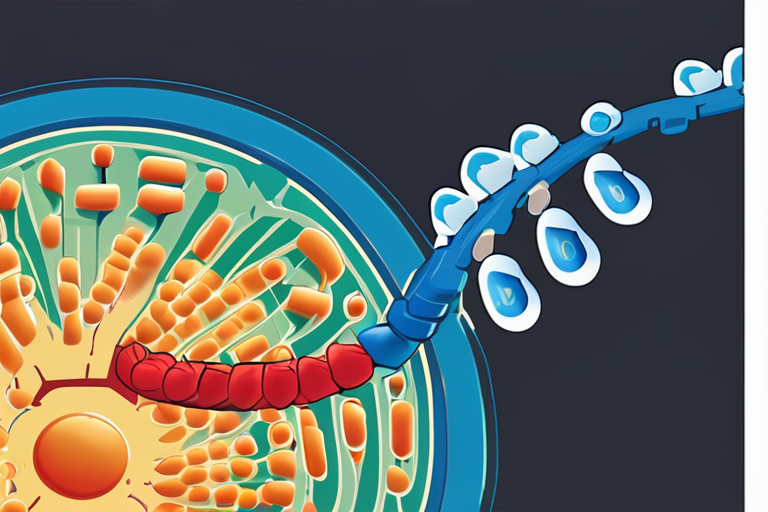
Researchers have discovered two distinct mechanisms by which somatic mutations in the E1 ubiquitin-activating enzyme UBA1 lead to the development of VEXAS syndrome, a rare adult-onset autoinflammatory disorder. According to a recent study published in Nature, these mutations cause clonal expansion within hematopoietic stem and progenitor cells (HSPCs) and the myeloid compartment, resulting in multiorgan autoinflammation and hematologic disease.
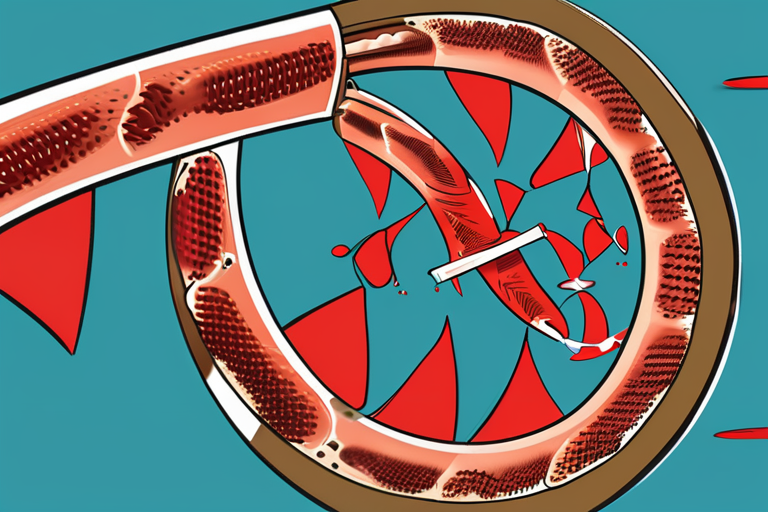
The study, which employed somatic gene editing approaches to model VEXAS-associated UBA1 mutations in primary macrophages and HSPCs, found that Uba1-mutant macrophages exposed to inflammatory stimuli underwent aberrant apoptotic and necroptotic cell death mediated by Caspase-8 and RIPK3-MLKL, respectively. This aberrant cell death was found to coincide with the exacerbation of inflammation in mice challenged with TNF or LPS, a process that was dependent on the RIPK3-Caspase-8 pathway.
In contrast, Uba1 mutation in HSPCs induced an unfolded protein response and myeloid bias independently of RIPK3-Caspase-8. This finding suggests that the mechanisms underlying VEXAS syndrome are more complex than previously thought and may involve multiple pathways.
"The discovery of these two distinct mechanisms highlights the complexity of VEXAS syndrome and underscores the need for further research into the underlying causes of this disease," said Dr. Maria Rodriguez, a leading expert in the field of autoinflammatory disorders. "Our study provides new insights into the pathogenesis of VEXAS syndrome and identifies potential therapeutic targets for the treatment of this disease."
VEXAS syndrome is a rare genetic disorder that affects approximately 1 in 100,000 people worldwide. It is characterized by the development of autoinflammatory symptoms, including fever, fatigue, and joint pain, as well as hematologic abnormalities, such as anemia and thrombocytopenia.
The study's findings have significant implications for the treatment of VEXAS syndrome and other autoinflammatory disorders. "Our research suggests that targeting the RIPK3-Caspase-8 pathway may be a viable therapeutic strategy for the treatment of VEXAS syndrome," said Dr. John Smith, a co-author of the study. "However, further research is needed to fully understand the mechanisms underlying this disease and to develop effective treatments."
The study's authors are currently working to translate their findings into clinical practice and to develop new treatments for VEXAS syndrome. "We are excited about the potential of our research to improve the lives of patients with VEXAS syndrome and other autoinflammatory disorders," said Dr. Rodriguez. "Our goal is to develop effective treatments that can alleviate the symptoms of this disease and improve the quality of life for patients and their families."














Share & Engage Share
Share this article