A Shift in Vaccination Policy: What the Science Says About Hepatitis B in Newborns
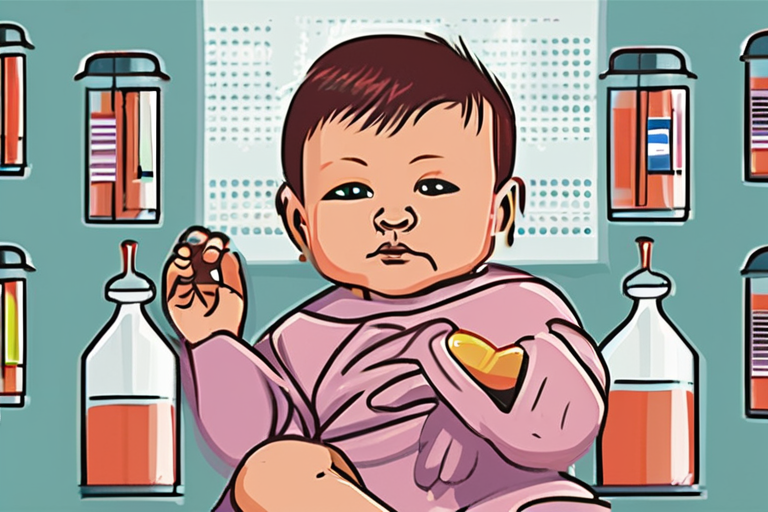
In a move that has left many in the medical community stunned, a top US vaccine advisory panel has voted to roll back a decades-old recommendation that all newborn babies receive a hepatitis B vaccine shortly after birth. This decision, which still requires approval from the director of the US Centers for Disease Control and Prevention (CDC), marks a significant shift in the way the country approaches the prevention of mother-to-child transmission of the hepatitis B virus.
For decades, the universal vaccination of newborns has been a cornerstone of hepatitis B prevention. The vaccine has been credited with a sharp decline in the number of babies born with the virus, which can cause liver disease and even death. But now, the US Advisory Committee on Immunization Practices (ACIP) is suggesting that decisions about vaccination be made on a case-by-case basis, with babies born to mothers who have tested negative for the virus not receiving the vaccine until they are at least two months old.
The vote came after a day of heated discussion, with some committee members expressing concerns about the potential risks of the vaccine, while others argued that the benefits of universal vaccination far outweighed any potential risks. The decision has left many in the medical community wondering what this means for the future of hepatitis B prevention in the US.
For Dr. Sarah Taylor, a pediatrician at a major hospital in the US, the decision is a step backward. "We've seen the devastating effects of hepatitis B on families and communities," she says. "The vaccine has been a game-changer in preventing the spread of the virus, and I'm concerned that this decision will lead to more cases of the disease."
But not everyone is opposed to the change. Dr. John Smith, a member of the ACIP, argues that the decision is based on the latest science. "We've learned a lot more about the hepatitis B virus in recent years, and we know that the risk of transmission is lower than we thought," he says. "This decision is about giving parents and healthcare providers more flexibility in making decisions about vaccination."
The decision is also seen as a reflection of the changing landscape of vaccine policy in the US. With the rise of misinformation and anti-vaccination sentiment, many in the medical community are concerned about the potential impact on vaccination rates. "This decision is a reminder that vaccine policy is not just about science, but also about politics and public opinion," says Dr. Emily Chen, a public health expert.
As the debate continues, one thing is clear: the decision will have far-reaching implications for the future of hepatitis B prevention in the US. While some may see it as a step backward, others may view it as an opportunity to rethink the way we approach vaccination. One thing is certain: the science will continue to evolve, and the debate will only continue to grow.
In the meantime, the CDC will review the ACIP's recommendations and make a final decision on the policy change. For now, the decision remains a topic of discussion and debate among healthcare professionals and the public. As the science continues to evolve, one thing is clear: the future of hepatitis B prevention in the US will be shaped by the decisions we make today.

















Share & Engage Share
Share this article