A Shift in Vaccination Policy: What the Science Says About Hepatitis B Vaccine Guidance for US Babies
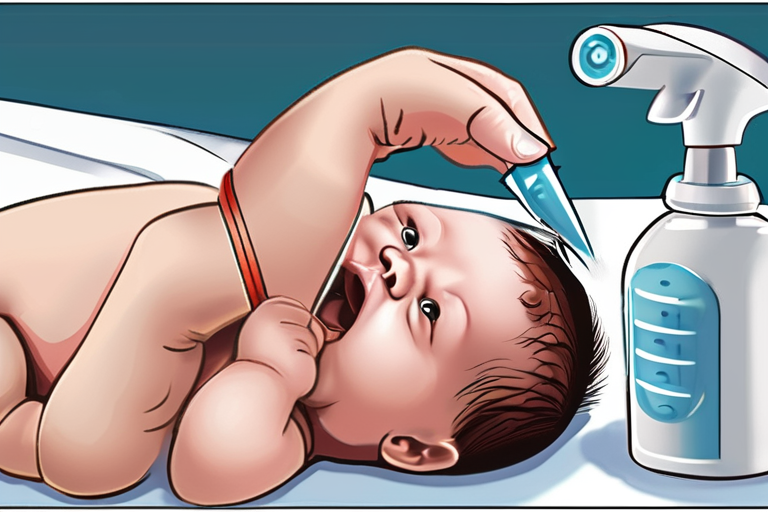
In a move that has left many in the medical community stunned, a top US vaccine advisory panel has voted to roll back a decades-old recommendation that all newborn babies receive a hepatitis B vaccine shortly after birth. The decision, made by the US Advisory Committee on Immunization Practices (ACIP), marks a significant shift in the country's approach to preventing the spread of the hepatitis B virus, which causes liver disease and can be transmitted from mother to child during birth.
For decades, the universal vaccination of newborns has been a cornerstone of the US's efforts to combat hepatitis B. The measure has been credited with a sharp decline in mother-to-child transmission of the virus, and has saved countless lives. But now, the ACIP has recommended that decisions about vaccinating newborns be made on a case-by-case basis, suggesting that babies who do not receive a birth dose of the vaccine be vaccinated no earlier than the age of two months.
The vote came after more than a day of discussion, during which time the panel grappled with the complexities of the issue. While some members argued that the current policy was too broad and did not take into account the individual circumstances of each mother and baby, others expressed concerns that rolling back the recommendation could lead to a resurgence of hepatitis B cases.
The decision is not yet final, as it must be approved by the director of the US Centers for Disease Control and Prevention (CDC) before it becomes official policy. But if implemented, it could have significant implications for the country's approach to preventing the spread of hepatitis B.
To understand the reasoning behind the ACIP's decision, it's essential to delve into the science behind hepatitis B and the current vaccination policy. Hepatitis B is a viral infection that can cause liver disease and is transmitted through bodily fluids, including blood and semen. The virus can be transmitted from mother to child during birth, and is a significant public health concern in the US, particularly among certain populations, such as African Americans and Asian Americans.
The hepatitis B vaccine has been widely available since the 1980s and has been shown to be highly effective in preventing the spread of the virus. The current policy of universal vaccination of newborns was implemented in the 1990s, and has been credited with a significant decline in hepatitis B cases.
But the ACIP's decision to roll back this policy is not without precedent. In recent years, there has been a growing trend towards more targeted and individualized approaches to vaccination, rather than blanket recommendations. This shift is driven in part by advances in medical technology, which have made it possible to identify individuals who are at high risk of contracting certain diseases.
Dr. Peter Hotez, a leading expert on vaccine policy and a member of the ACIP, argues that the decision to roll back the hepatitis B vaccination policy is a necessary step towards a more nuanced and effective approach to public health. "We're moving away from a one-size-fits-all approach to vaccination, and towards a more targeted approach that takes into account the individual circumstances of each mother and baby," he says.
But not everyone agrees with the ACIP's decision. Dr. Paul Offit, a pediatrician and vaccine expert, argues that the current policy is effective and should not be changed. "We've seen a significant decline in hepatitis B cases since the introduction of the vaccine, and there's no evidence to suggest that rolling back the policy will have any benefits," he says.
As the debate over the ACIP's decision continues, it's clear that the implications will be far-reaching. If implemented, the new policy could lead to a resurgence of hepatitis B cases, particularly among certain populations. On the other hand, it could also lead to a more targeted and effective approach to public health, one that takes into account the individual circumstances of each mother and baby.
Ultimately, the decision will depend on the director of the CDC, who will review the ACIP's recommendation and make a final decision. But one thing is clear: the science behind hepatitis B and the current vaccination policy is complex, and requires a nuanced and thoughtful approach.
As the medical community continues to grapple with the implications of the ACIP's decision, one thing is certain: the future of hepatitis B vaccination policy will be shaped by the latest developments in science and technology. And it's up to us to stay informed and engaged, as we navigate this critical issue and work towards a healthier future for all.
























Share & Engage Share
Share this article